The World Health Organization (WHO) was founded in 1948 during the flush of idealistic enthusiasm that followed the ending of the Second World War. Its constitution is notable for its scope and breadth, setting out 22 functions for WHO covering almost every conceivable activity linked to the promotion of health. Health is broadly defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”.
Much like the UN itself, most people agree that if WHO did not exist it would be necessary to invent it. A topical example is the recent Ebola outbreak in West Africa, declared by WHO to be an international public health emergency. Even if there have been some criticisms about the way WHO has handled it, how would the international response be led and coordinated in the absence of a body such as WHO? Combatting the international spread of infectious diseases remains one of the organisation’s most important functions. Its authority to do so stems from the first international convention on public health in 1892, related to the spread of cholera. And of course the eradication of smallpox in the 1970s is widely regarded as one of WHO’s greatest achievements.
In addition to this high-profile work, WHO performs a number of essential but less visible functions of importance to global health. It helps to set norms and standards to guide healthcare work around the world, using its unique position to draw on the knowledge of leading experts worldwide. For example, in light of the latest evidence, WHO regularly updates its treatment guidelines on HIV/AIDS, malaria and other diseases.
Developing countries, particularly those with weak healthcare systems, also benefit from WHO’s technical support. With 150 country and six regional offices, it should be well placed to offer technical assistance to those that need it. For many countries, the issuing of new treatment guidelines is helpful, but working out how to implement them is another matter. The support of WHO, as well as other agencies, could be invaluable in helping them to do so.
So could WHO do better? This is the hard part. WHO has about 7,000 permanent staff – only one quarter of whom are based in Geneva – and many thousands more contracted staff around the world. WHO is by some distance the largest UN specialised agency, other than the World Bank. It has an annual budget of $2bn, of which just a quarter comes from member statemandatory contributions. The remainder comes from voluntary contributions from high-income countries, usually earmarked for particular activities they favour, and increasingly from foundations. In 2013, the single largest contributor to WHO was the Bill and Melinda Gates Foundation, which gave more than $300m.
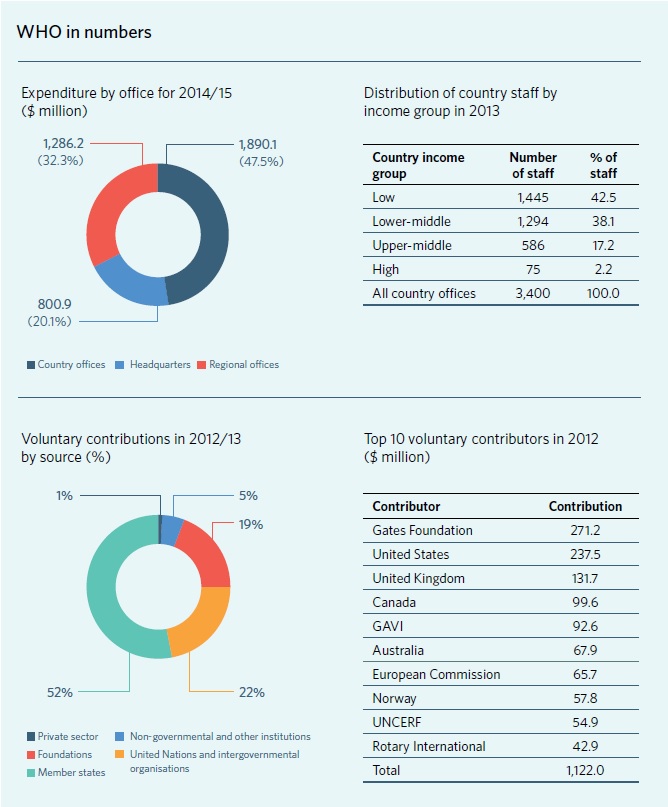
This financing model makes WHO exceedingly complex to manage – it is estimated that one third of its budget goes on management and administration. And it undermines WHO’s existing governance structure because it is the voluntary funders, not WHO member states collectively, that mainly determine how resources are directed.
There is also no stable funding base for WHO’s important regulatory and normative activities, many of which are not attractive to funders who prefer the immediate and visible results of project work. As part of its current reform programme that began in 2010, WHO is attempting to square this circle through a “financing dialogue” with its voluntary contributors, aimed to persuade them to direct their funding in accordance with the budget approved by WHO’s governing body. But it remains to be seen whether this can really change the underlying contradictions in the way WHO is financed.
Moreover, WHO is unique among UN agencies in that it is the regional member states that elect the directors of the six regional offices. Each regional director is effectively beholden to the regional member states, not to their nominal chief, the Director-General, currently Margaret Chan. In turn, this means that she can only seek to persuade her six regional directors to act as she wants – she cannot exert her authority or replace them if they fail to perform. As a result, the common saying is that there is not one but seven WHOs. And this is another reason why WHO’s administrative costs are so high.
But it is precisely because of this supposedly democratic structure and the unusual financing model that WHO’s reform programme fails to address important questions in any meaningful way. The politics of WHO means that it is very difficult to discuss whether the organisation actually needs 150 country and six regional offices to perform its functions. Is there not possibly some fat there? Could these resources be put to more effective use elsewhere? Is the seven WHOs structure immutable?
The large majority of WHO’s member states pay far less in contributions than they get back in terms of benefits. Thus all low- and middle-income countries together annually pay in a little over $60m while it is they who mainly benefit from the $1.3bn WHO spends each year in its country and regional offices alone. In such circumstances these countries can hardly be blamed for not looking a gift horse in the mouth. Moreover, WHO’s regional and country office structure opens up opportunities for government officials to obtain employment on UN salary scales – an attractive incentive for any country that hosts WHO.
For their part, the high-income countries and other voluntary contributors, while footing most of the bill, and paying lip service to the need for reform, seem happy with this way of managing WHO, whatever its faults and inefficiencies. It is therefore not surprising that there is reluctance on the part of member states to question seriously the status quo.
So can WHO be reformed? The main message from this analysis is that the political preconditions for any fundamental reform of WHO do not exist. The current WHO reform programme meanders on but not in a way that will transform the organisation – it is more about adaptation to changing external circumstances. Some influential voices are therefore asking whether there are other organisations that could do some or all of WHO’s work better and more efficiently.
Charles Clift is a Senior Consulting Fellow at the Centre on Global Health Security at Chatham House and recently published “What’s the World Health Organization For?”, a report offering recommendations for serious reform of WHO’s core functionality, governance and financing